Welcome to the Be Well Blog
My little corner of the internet...
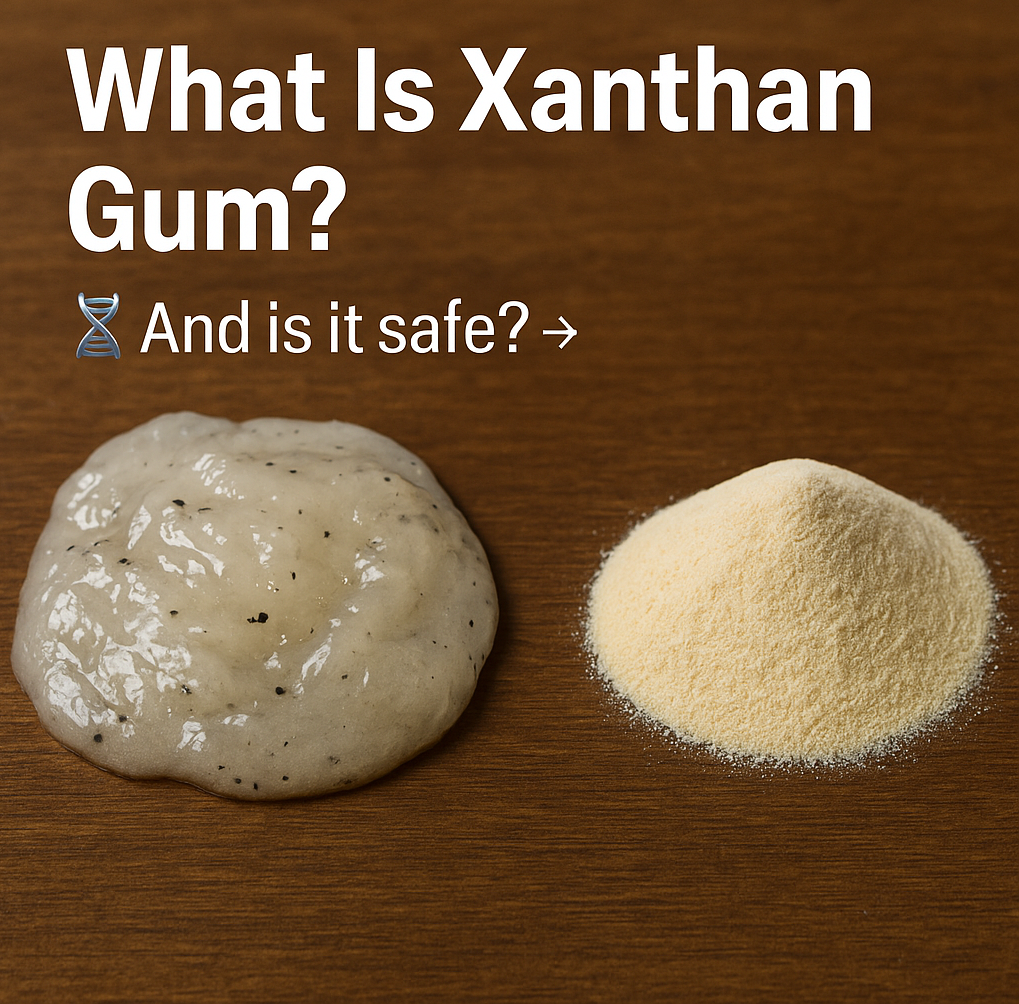
Xanthan gum is a polysaccharide produced when the bacterium Xanthomonas campestris ferments sugars (most often from corn, but sometimes soy, wheat, or other plant sources). After fermentation, the sticky “goo” is purified, dried, and milled into a fine powder. That’s xanthan gum and it’s widely used as a thickener, stabilizer, emulsifier, and binder in foods like salad dressings, sauces, gluten-free breads, and dairy substitutes. Because of its ability to withstand acid, heat, and salt, it’s especially useful in creating consistency and texture in processed foods. Is It Safe and for Whom? For most people, xanthan gum is considered safe in the small amounts typically used in food. But here’s a more nuanced look: Regulatory status: In the U.S., xanthan gum is classified as GRAS (“Generally Recognized as Safe”) by the FDA. In Europe, EFSA has also evaluated it (E 415) and found no concerns for the general population, even with long-term exposure. Toxicity / long-term effects: Animal studies at very high doses showed minimal adverse effects and no evidence of toxicity or genetic damage. The phrase used in assessments: “no adverse effects observed up to the highest dose tested.” Digestive side effects: At very large doses, xanthan gum may cause gas, bloating, or softer stools. Most reports of discomfort occur at intakes around 15 grams per day far more than you’d get from normal processed foods. Effect on gut bacteria: Newer studies show that some gut microbes can break down xanthan gum, producing short-chain fatty acids that may benefit gut health. Research also suggests the human microbiome has adapted to digest xanthan gum, creating new “food chains” in the gut. Blood sugar and cholesterol effects: Early research hints that xanthan gum may modestly lower blood sugar after meals and reduce cholesterol, though human data is limited. Allergies and sensitivities: Since it’s often derived from corn, soy, wheat, or dairy, people with severe allergies should be cautious. Those with sensitive digestion (IBS, gut disorders) may notice symptoms if intake is high. Infants and special populations: Thickened baby formulas using xanthan gum have been linked to necrotizing enterocolitis (NEC) in premature infants, so it should be avoided in that context. There is limited data on safety during pregnancy and breastfeeding. Bottom line: For most healthy adults, the small amounts in food are unlikely to cause harm. Concerns arise mainly with very high intake or in people with sensitivities. Why It Matters Now and What’s New? Microbiome interaction: A recent study found a gut bacterium (from the Ruminococcaceae family) can break xanthan gum into smaller molecules, which other bacteria then consume. This shows xanthan gum actively shapes the gut microbiome. Unique structure: Unlike many dietary fibers, xanthan gum has a distinct structure, meaning it interacts differently with microbes. Emulsifier research: Some studies on emulsifiers suggest possible links to gut inflammation and metabolic changes in lab models. While not proven in humans, it highlights the need for more study. What to Watch For & How to Be Intentional If you experience bloating or digestive issues, check labels xanthan gum could be a factor. If you have allergies to corn, wheat, soy, or dairy, verify the source when possible. Don’t assume gluten-free always equals healthy many gluten-free products rely heavily on xanthan gum. In cooking, consider alternatives like guar gum, psyllium husk, chia, or flax though each has its own quirks. The takeaway: For most, xanthan gum is harmless in small amounts. But awareness helps you make more intentional food choices especially if you have sensitivities.

Understanding Time Anxiety Chris Guillebeau, in his book Time Anxiety: The Illusion of Urgency and a Better Way to Live, delves into the root causes of our time-related stress. He explains that: Time anxiety stems from unrealistic expectations and misaligned priorities, not from a genuine lack of time. We often feel overwhelmed by incomplete tasks and unmet goals, leading to a perpetual state of urgency. This constant pressure can leave us feeling overstimulated and exhausted, impacting our mental and physical health. The Perils of Overscheduling Dan Martell's Buy Back Your Time emphasizes the importance of reclaiming control over our schedules. He suggests: Identifying and outsourcing low-value tasks to focus on what truly matters. Creating a schedule that aligns with personal values and goals, rather than filling every moment with activities. Overscheduling can lead to: Chronic stress and fatigue, Weakened immune system and increased risk of illness.Reduced productivity and creativity. The Link Between Perfectionism and Time Anxiety Perfectionism often fuels time anxiety, as individuals set unattainable standards and overcommit to tasks. This can result in: Heightened anxiety and fear of failure. Procrastination due to fear of not meeting expectations. Difficulty in prioritizing tasks effectively. Recognizing and addressing perfectionist tendencies is crucial in alleviating time anxiety. Embracing Self-Care for Holistic Well-Being Prioritizing self-care is essential in combating time anxiety and its associated effects. Holistic self-care practices include: Physical Health: Regular exercise, balanced nutrition, and adequate sleep. Emotional Wellness: Mindfulness, gratitude practices, and emotional regulation. Mental Clarity: Engaging in activities that stimulate the mind and foster creativity. Saying no isn’t selfish—it’s an act of self-respect. When you say yes to everything, you're often saying no to your own health, peace, and priorities. But saying no doesn’t have to burn bridges—it can build better boundaries. Here’s how to do it gracefully and effectively: 1. Be Clear, Not Cruel You don’t have to over-explain or apologize excessively. Try this: “I’m focused on fewer commitments right now to protect my energy, but I appreciate you thinking of me.” 2. Use the “Soft No + Redirect” Offer support without taking on the full burden. Example: “I can’t lead that project this time, but I’m happy to review it or offer feedback.” 3. Delay Your Response Give yourself space to assess your capacity before committing. Say: “Let me check my schedule and get back to you.” (Then practice saying no if needed.) 4. Honor Your Values Saying no to what’s misaligned frees you to say yes to what matters most—your health, your peace, your vision. Saying No Is Self-Care for the Soul When you learn to say no with kindness but firmness, you reduce stress, improve your relationships, and reclaim your time. It’s a power move—for your body, brain, and business. Need help learning how to say no and still feel like a good friend, partner, or leader? Let’s work on that together. Coaching can help you create strong, loving boundaries that honor who you are becoming. By integrating these practices, individuals can enhance resilience, reduce stress, and improve overall quality of life. Take the First Step Towards Reclaiming Your Time If you're feeling overwhelmed by time anxiety and the pressures of perfectionism, know that you're not alone. Our coaching services are designed to help you: Identify and realign your priorities. Develop personalized strategies to manage your schedule effectively. Cultivate self-compassion and resilience. Contact us today to begin your journey towards a balanced and fulfilling life. With Love Be Well Susan Lee

I will boldly admit this was a stumbling block for me since childhood, and if we are honest, isn't that where all self-limiting beliefs begin? It takes work and reprogramming negative self-talk to release this inner narrative. 'When you focus on how unfair life seems and compare yourself to others, you are draining your motivation and keeping yourself from moving forward. It becomes a self-fulfilling prophecy. You are failing because of your chronic habit of comparing yourself. The first step is accepting the truth: life isn’t fair. It’s just not. The reality is you can’t control another person’s success, luck, or timing in life. The only thing you can control is what you do with the example others set and the actions you take next." Mel Robbins The Hidden Costs of Comparison Physical Toll: How Comparison Affects Your Body Comparison isn’t just a mental exercise—it has direct effects on your body. Chronic stress from comparing yourself to others can lead to: Increased cortisol levels, which can cause weight gain, fatigue, and inflammation. Sleep disturbances, making it harder to recover and perform well in your daily life. Weakened immune function, leaving you more susceptible to illness. Adrenal fatigue, especially if you are constantly feeling "behind" and pushing yourself beyond your limits. The stress response triggered by comparison keeps your body in a constant state of fight-or-flight, which can lead to burnout and even chronic health conditions over time. Emotional and Psychological Damage Comparison not only affects your body but also erodes your mental and emotional well-being: Anxiety and depression – Constantly measuring yourself against others can make you feel inadequate and hopeless. Low self-esteem – When you focus on what others have, you may fail to see your own strengths and progress. Perfectionism and procrastination – Feeling like you're never "good enough" can paralyze you from taking action. Resentment and bitterness – Comparison can make you feel envious or unfairly treated, damaging relationships and personal growth. When comparison turns into self-judgment, it reinforces a negative cycle that keeps you stuck. Instead of using others' success as inspiration, you become trapped in a loop of self-doubt. Breaking Free: How to Stop Comparing Yourself to Others The good news? Comparison is a habit, and habits can be changed. Here are some research-backed strategies to help you shift your mindset and reclaim your motivation: 1. Reframe Your Perspective Instead of seeing others’ success as a threat, view it as proof of what’s possible. Psychological research suggests that adopting a growth mindset—the belief that your abilities can be developed—leads to greater success and happiness. If someone has achieved something you admire, ask: What can I learn from them? Use their journey as inspiration rather than as a measurement of your own worth. 2. Limit Your Exposure to Triggers Social media is a major source of unhealthy comparison. Studies show that excessive social media use can lower self-esteem and increase anxiety. Take breaks from scrolling. Follow accounts that inspire rather than trigger self-doubt. Remind yourself that people often showcase their highlights, not their struggles. 3. Focus on Your Own Progress Comparison steals your joy because it makes you measure yourself against someone else’s timeline. Instead, track your own growth. Keep a journal of small wins and milestones. Set personal goals based on where YOU want to be, not where someone else is. Celebrate your progress, no matter how small. 4. Practice Gratitude and Self-Compassion Research shows that gratitude can reduce stress and increase happiness. Instead of focusing on what you lack, shift your attention to what you have. Write down three things you’re grateful for every day. Acknowledge your strengths and efforts rather than just results. Be kind to yourself when you make mistakes. 5. Take Action Instead of Overthinking Comparison often leads to paralysis. The more you dwell on where you “should” be, the less action you take. Break this cycle by focusing on small, daily actions that align with your goals. Instead of saying, I wish I had what they have, ask What’s one thing I can do today to improve my situation? Shift from comparison to creation—build something meaningful in your own life. Final Thoughts Comparison is a thief of joy, motivation, and well-being. But you don’t have to stay trapped in the cycle. By shifting your perspective, limiting comparison triggers, focusing on personal growth, and practicing self-compassion, you can reclaim your energy and start moving forward. The reality is life isn’t fair—but that doesn’t mean you can’t create a life that feels fulfilling and aligned with your own path. The only thing you can control is what you do next. So, what’s your next step? If you're ready to create a clear vision for your future self and step into the life you truly want, reach out—I’d love to help you make it a reality! With Love Be Well Susan Lee

As we conclude Dry January, many individuals may struggle to maintain their goal of reducing alcohol consumption. Having grown up with an alcoholic parent, I have witnessed the detrimental effects it can have on relationships and the lifespan of family members. Reflecting on my own teenage dependency and the social pressure to drink, I understand how easily one can lose control of their priorities and goals. I hope I have imparted to our children the importance of maintaining a healthy relationship with alcohol, as it is crucial to leading a fulfilling life. Additionally, I want them to know that it is perfectly acceptable to not drink at all; being intoxicated does not always equate to having fun and more time than not, results in hurtful and destructive consequences for friends and family. Alcohol consumption has far-reaching effects on various aspects of human health, influencing the brain, liver, and the aging process. Understanding these impacts, along with statistics on alcohol-related health issues and strategies for fostering a healthier relationship with alcohol, is crucial for informed decision-making. Effects of Alcohol on the Brain Alcohol interferes with the brain’s communication pathways, affecting how the brain processes information. Chronic, heavy alcohol consumption can lead to alcohol-related dementia (ARD), characterized by cognitive deficits and impairments in professional and social life. Research indicates that such consumption leads to degeneration and demyelination of the corpus callosum, a critical brain structure responsible for communication between the two hemispheres. Impact on the Liver The liver plays a central role in metabolizing alcohol. Excessive drinking can cause inflammation known as alcoholic hepatitis, which may progress to irreversible damage, including liver enlargement, scarring (cirrhosis), and an increased risk of liver cancer. Individuals genetically predisposed to liver conditions are at heightened risk when consuming alcohol. Alcohol and Aging Alcohol can accelerate the aging process by affecting vital organs. Heavy drinking is associated with liver diseases such as cirrhosis and can contribute to other health issues that expedite aging. Additionally, aging slows the body’s ability to metabolize alcohol, causing it to remain in the system longer and potentially leading to increased sensitivity and adverse effects. Alcohol-Related Health Statistics Between 2016 and 2021, the United States saw a significant increase in deaths from excessive alcohol use, rising from an annual average of 137,927 to 178,307—a 29.3% increase. In 2022 alone, alcohol-impaired driving fatalities accounted for 13,524 deaths, representing 32% of all driving fatalities. Strategies for a Healthier Relationship with Alcohol To foster a healthier relationship with alcohol, consider the following strategies: • Set Personal Limits: Define specific days or occasions for alcohol consumption to avoid habitual drinking. • Choose Low-Alcohol Alternatives: Opt for beverages with lower alcohol content to reduce overall intake. • Engage in Alternative Activities: Plan social events that don’t center around alcohol, such as physical activities or cultural outings. • Mindful Drinking: Be conscious of the reasons behind drinking and assess whether it’s necessary in each situation. • Seek Support: Join groups or programs that promote sobriety or moderate drinking habits. Understanding the multifaceted effects of alcohol empowers individuals to make informed choices, promoting better health and well-being. Alcohol and Weight Management Regular alcohol consumption can hinder weight management efforts in several ways: • High Caloric Content: Alcoholic beverages are often high in calories, contributing to weight gain. • Increased Appetite and Poor Food Choices: Alcohol can increase appetite and lead to cravings for unhealthy foods, further contributing to weight gain. • Metabolic Impact: Alcohol provides empty calories, heightens cravings, and may slow down metabolism, making weight loss more challenging. Reducing alcohol intake can support weight loss efforts by decreasing calorie consumption and minimizing negative impacts on metabolism. Habit-Forming Concerns with Social Drinking Social drinking can lead to habit formation due to the repetitive cycle of cues (social events), routines (drinking), and rewards (social enjoyment). This habit loop reinforces the behavior, making it challenging to reduce alcohol consumption. Implementing these practices can lead to improved health outcomes and a more balanced lifestyle. Understanding the multifaceted effects of alcohol empowers individuals to make informed choices, promoting better health and well-being. Alcohol consumption significantly impacts various aspects of health, including weight management and the formation of social drinking habits. Understanding these effects and implementing strategies to manage alcohol intake can promote better health outcomes. The Effects of Alcohol on Your Brain – By Dr. Daniel Amen "Many people think of alcohol as a harmless way to relax or socialize, but the truth is that it has significant effects on your brain—many of which can be damaging. Alcohol reduces blood flow to the brain, leading to lower activity in critical areas responsible for decision-making, memory, and emotional regulation. Over time, regular drinking can shrink the hippocampus, the brain’s memory center, increasing the risk of dementia. It also disrupts neurotransmitters like dopamine and serotonin, which can contribute to depression and anxiety." Even moderate alcohol use can impair judgment and increase impulsivity, making it harder to make healthy choices. And if you’re trying to optimize your brain health, alcohol is working against you. The good news? Your brain has the ability to heal. Reducing or eliminating alcohol can lead to better focus, improved mood, and increased brain function. Your brain is your greatest asset—protect it! If you want to change your relationship with Alcohol, lets visit about what that would look like as part of an overall plan for a healthier you! With Love Be Well Susan Lee

Achieving sustainable health and wellness often begins with setting clear, actionable goals. But goal-setting isn’t just about deciding what you want to achieve—it’s about creating a mindset and structure that supports you throughout the process. A holistic approach to health takes into account not just physical goals, but also emotional, mental, and spiritual well-being. By fostering balance in all areas of your life, you’re more likely to stick with your goals, experience lasting success, and cultivate a healthy lifestyle you truly enjoy. Why Goal Setting Is Important for Health? When we think about health, many people focus solely on losing weight or getting fit. However, health encompasses much more than just the physical body. Setting goals gives you direction, helps you prioritize your health, and motivates you to follow through on positive habits. Without clear goals, it’s easy to lose track or fall back into old patterns. According to Dr. Edwin Locke, a psychologist renowned for his work on goal-setting theory, specific and challenging goals lead to better performance than vague or easily achievable ones (Locke & Latham, 2002). Start with the ‘Why’ – Align Your Goals with Your Values Before setting your health goals, take a moment to reflect on your deeper motivations. Why do you want to achieve these goals? Is it to feel more energetic, improve your mood, enhance your physical strength, or something else? When you connect your goals to your core values and deeper purpose, you create a more meaningful path forward. For instance, if your goal is to eat healthier, your motivation may be to improve your long-term health or increase your energy to enjoy life with your family. Having this purpose in mind will help sustain your commitment. Set SMART Goals: Specific, Measurable, Achievable, Relevant, and Time-Bound One of the most effective ways to set goals is by using the SMART framework. This approach ensures your goals are clearly defined and realistic. Here’s a breakdown: • Specific: What exactly do you want to achieve? Instead of “I want to eat better,” try “I want to eat five servings of vegetables a day.” • Measurable: How will you track your progress? If you’re aiming for 5 servings of vegetables, keep a food journal or use an app to track your intake. • Achievable: Is your goal realistic given your current situation? If you’re new to exercise, a goal of working out 5 days a week might not be sustainable. Instead, aim for 2 or 3 sessions and gradually build. • Relevant: Is the goal important to you and aligned with your values? Make sure it’s something that resonates on a deeper level. • Time-Bound: Set a deadline for your goal. For example, “I’ll be able to run 2 miles in 8 weeks.” By following this method, you ensure that your goals are clear, attainable, and focused on making real progress. The Power of Small, Consistent Habits Setting large, lofty goals can feel overwhelming, especially when they require a drastic shift in your lifestyle. Instead of trying to overhaul everything at once, focus on small, sustainable changes. Start by introducing one new healthy habit at a time. Whether it’s drinking an extra glass of water each day, taking a 10-minute walk after lunch, or reducing sugar intake, these small actions add up over time. As James Clear, author of Atomic Habits, suggests, “You do not rise to the level of your goals. You fall to the level of your systems.” Small habits, when built over time, create a strong foundation for larger transformations. Addressing Mental and Emotional Health Health is not just about the body—it’s about how you think and feel, too. Emotional and mental well-being play a huge role in whether or not you achieve your goals. If stress, anxiety, or negative self-talk holds you back, those issues need to be addressed. Incorporating practices like mindfulness, meditation, and journaling can help you stay grounded and focused. By nurturing your mental health, you enhance your resilience, which makes it easier to handle challenges and stay committed to your goals. Building a Support System Success doesn’t happen in isolation. Whether it’s a workout buddy, a coach, a friend, or a community group, having people to support you can significantly increase your chances of success. Surrounding yourself with positive influences holds you accountable, offers encouragement, and makes the journey more enjoyable. As health coach and author, Dr. Deepak Chopra, points out, “When you join a community that supports your goals, you begin to tap into a collective energy that propels you forward.” Reframe Setbacks as Opportunities One of the biggest challenges in achieving health goals is the inevitable setback. You might miss a workout, indulge in unhealthy food, or slip back into old habits. Instead of letting these moments derail your progress, reframe them as learning opportunities. Every setback is a chance to assess what happened, make adjustments, and continue moving forward. As Brene Brown, a researcher on vulnerability and resilience, explains, “We don’t have to be perfect to be worthy of success; it’s through our imperfections that we grow.” Celebrate Your Wins It’s easy to get caught up in striving for the next goal without taking time to appreciate how far you’ve come. Celebrate your progress, no matter how small it may seem. If you successfully met your weekly exercise goal or ate more fruits and vegetables, take a moment to acknowledge your hard work. Celebrating victories boosts motivation and reinforces the positive behaviors you’re cultivating. Stay Flexible and Adaptable Life isn’t static, and neither should your goals be. Flexibility is key to maintaining long-term success. Your circumstances, needs, and priorities will change, and so will your goals. Instead of being rigid, embrace the idea of adjusting your goals as needed. This will allow you to stay committed to your well-being while adapting to life’s inevitable ebbs and flows. A Holistic Approach: Integrating Mind, Body, and Spirit Ultimately, a holistic approach to goal setting and health means addressing all aspects of your well-being. Physical health is important, but so is your mental, emotional, and spiritual health. Practices such as yoga, meditation, deep breathing, and even spending time outdoors can enhance your sense of balance and wholeness. By integrating all of these dimensions, you create a robust, sustainable foundation for your goals, ensuring that they’re not just short-term fixes but lifelong changes. Conclusion Goal setting is more than just a task—it’s an ongoing process of growth, learning, and self-discovery. By taking a holistic approach to health, setting specific goals, and committing to small, consistent changes, you can create a lifestyle that supports your mind, body, and spirit. And remember, health is a journey, not a destination. Be patient, stay consistent, and embrace the process. Quick Summary: • Start with a purpose: Connect your health goals to your values and deeper motivations. • Use SMART goals: Ensure goals are Specific, Measurable, Achievable, Relevant, and Time-Bound. • Small habits, big results: Introduce small, sustainable changes for lasting transformation. • Focus on mental health: Incorporate practices like mindfulness and journaling to stay grounded. • Build a support system: Surround yourself with positive influences to stay motivated. • Learn from setbacks: Reframe challenges as opportunities for growth. • Celebrate progress: Acknowledge every victory to stay motivated. • Stay adaptable: Be flexible and adjust your goals as life changes. • Holistic approach: Integrate mind, body, and spirit for comprehensive well-being. For more personalized health coaching and tips, visit susanleeinc.com . Let’s work together to make your health goals a reality! With Love Be Well Susan Lee

I wanted to explore a new direction with this blog, drawing directly from a compelling Brain Health course I recently completed. Alzheimer's and Dementia hold a special place in my heart, as my mother faced health challenges last year. With the assistance of a neuropathic chiropractor and my mother's own resolve to heal, she embarked on altering her diet and lifestyle to observe any improvements. My research into Covid Dementia and the virus's varied effects on individuals resonated with me, having managed my own brain health following a prolonged struggle with Covid. I recognized how it could instigate an immune response against various body parts. Embracing this new lifestyle, my mom significantly reduced sugar and other inflammatory foods from her diet and has witnessed considerable improvement. The most valuable advice I can offer is to have a health advocate by your side when interacting with the medical community. This person should be capable of posing challenging questions and resisting protocols that seem incorrect or inconsistent with your findings. Indeed, conducting personal research is essential, as we are all unique and do not conform to a universal health protocol. Regrettably, our healthcare system does not cater to individualized care unless you consult a functional medicine doctor who aims to identify the underlying cause of your health concerns. This is my second key insight: seeking second opinions is not just recommended; it should be actively encouraged. There is a lot of technical discussion in this blog but also real sound advice and most important HOPE. We have the ability to choose how we enter our senior years, and it all starts now. With Love, Be Well Susan Lee Day 1 Summary from Alzheimer’s is Now Optional Welcome to the New Era of Brain Health Dr Dale Bredesen: KEY TAKEAWAYS The Evolutionary Basis of Neurodegenerative Diseases: Human evolution prioritized performance over durability, leaving neural subsystems vulnerable to conditions like Alzheimer’s, Parkinson’s, ALS, and macular degeneration. Understanding Alzheimer’s Pathology: Neurodegenerative diseases result from structural and molecular changes in the brain, such as amyloid plaques, tau tangles, and chronic inflammation, which are protective responses to various stressors. Cognitive Resilience and Brain Modes: The brain shifts between growth (connection) and defense (protection) modes, with neurodegenerative conditions characterized by the brain in chronic “defense” mode. Addressing root causes like inflammation, pathogens, and nutrient deficiencies can help the brain regrow and reverse cognitive decline. The Role of Precision Medicine: A comprehensive approach that identifies and addresses multiple drivers of neurodegenerative diseases—such as inflammation, glycotoxicity, and environmental toxins—can make cognitive decline preventable and reversible. The key is identifying the unique drivers for each individual. Nutrition and Lifestyle Strategies: Practical interventions, including the KetoFLEX 12/3 dietary plan (a plant-rich, mildly ketogenic diet), can improve brain health and reduce the risk of cognitive decline. The Power of Early Detection: New blood tests, such as P-tau217 and other biomarkers, enable early detection of brain health issues, making it possible to intervene before significant cognitive decline occurs. Drugs Mentioned ● Lecanemab: A drug mentioned for its limited ability to slow cognitive decline in Alzheimer’s patients, though it does not improve symptoms or reverse the disease. Tests Mentioned Blood Tests for Early Detection: ● P-tau217 and P-tau181: Biomarkers that help detect early signs of Alzheimer’s disease. ● Aß42 to Aß40 Ratio: Provides information on whether amyloid plaques are forming, indicating an inflammatory state in the brain. ● Neurofilament Light (NFL): Indicates neuronal damage from various causes, such as head injury, vascular issues, or degenerative diseases. ● Glial Fibrillary Acidic Protein (GFAP): Detects ongoing inflammation and repair activity in the brain. Traditional Tests: ● PET Scans: Used for diagnosing Alzheimer’s by detecting amyloid plaques in the brain. ● Spinal Taps: Previously standard for Alzheimer’s diagnosis, though less practical due to their invasiveness. These advancements in blood tests and their ability to monitor brain health represent a significant improvement in detecting and managing neurodegenerative diseases. Day 2 Summary from Alzheimer’s is Now Optional The Science and Strategies that Work to Reverse Alzheimer’s KEY TAKEAWAYS Translating Research into Action: Today’s lesson focuses on how to apply knowledge about neurodegenerative diseases into actionable programs for prevention and reversal, showcasing real-world success stories of patients who have dramatically improved through targeted protocols. The Impact of Neurodegenerative Diseases: Alzheimer’s is the third leading cause of death in the United States, and nearly everyone is affected, either personally or through family and friends, by neurodegenerative diseases like Alzheimer’s, Parkinson’s, or cognitive issues post-COVID. Case Study Successes: ● A 65-year-old woman with posterior cortical atrophy regained her ability to read, use a computer, and perform brain training after following the protocol for 15 months, with significant improvements in brain volume and cognitive function. ● A 66-year-old man reversed high fasting insulin, inflammation, and other markers, leading to a 23% increase in gray matter volume and restored ability to work full-time. Understanding Brain Function and Degeneration: ● The parietal lobe manages motor programs, calculations, and understanding visual information. ● The occipital lobe processes vision. ● The temporal lobe, especially the hippocampus, is critical for memory and neuroplasticity. ● The frontal lobes govern executive function, planning, and behavior. Drivers of Neurodegeneration: Alzheimer’s and similar conditions result from an imbalance of demand (inflammation, toxicity) versus supply (blood flow, oxygenation, hormones, nutrients, mitochondrial function). Chronic illnesses, including Alzheimer’s, are signaling imbalances similar to osteoporosis or cancer. For example, in a normal brain the signals for growth/connection and defense/contraction are balanced, but in neurodegenerative diseases an imbalance between these leads to degeneration. APOE Genetic Risk and Implications: ● APOE4, the most common genetic risk for Alzheimer’s, significantly increases the likelihood of developing the disease but can be mitigated with early action. ● New drugs and genetic insights offer the potential for turning APOE4 effects into protective APOE3-like impacts. Role of Lifestyle and Biomarkers: ● Key metrics such as fasting insulin, inflammation (hs-CRP), homocysteine, and vitamin D3 levels are critical markers to address for improving brain health. ● Optimizing metabolism and reducing inflammatory factors directly support cognitive function and brain volume. Advances in Genomic Testing: Tools like Nebula, Apollo Health, 3X4 Genetics, and IntellxxDNA allow individuals to assess their genetic risks and create personalized prevention strategies. The Future of Brain Health: Early detection and intervention can prevent and reverse neurodegenerative diseases, marking the 21st century as a turning point where conditions like Alzheimer’s can become preventable for future generations. Drugs Mentioned ● Experimental APOE4-Modifying Drug: A drug under development to reduce the effects of APOE4 and make it behave more like the protective APOE3 variant. This drug is not yet approved but has been developed in collaboration with UCLA. Tests Mentioned Genetic Tests for APOE Status: ● Knowing your APOE4 status is highlighted as a critical step for understanding Alzheimer’s risk. ● Platforms mentioned for genetic testing include Nebula, Apollo Health, 3X4 Genetics, IntellxxDNA, and Function Health. Biomarker Tests: ● Fasting Insulin: High levels indicate insulin resistance, which is linked to cognitive decline. ● hs-CRP (High-Sensitivity C-Reactive Protein): A marker for inflammation; elevated levels are a risk factor for neurodegeneration. ● Homocysteine: Elevated levels are associated with a higher risk of cognitive decline. ● Vitamin D3 Levels: Important for synapse formation and overall brain health; low levels are detrimental. Day 3 Summary from Alzheimer’s is Now Optional Alzheimer's Phases and How to Reverse Cognitive Decline KEY TAKEAWAYS The Four Phases of Alzheimer’s: 1. Phase 1 (Asymptomatic): No noticeable symptoms. Early changes are detectable as early as your 20s or 30s through blood tests like p-tau217, PET scans, or spinal taps. 2. Phase 2 (Subjective Cognitive Impairment, SCI): Noticeable brain fog or memory issues, lasting up to 10 years. Highly reversible with intervention. 3. Phase 3 (Mild Cognitive Impairment, MCI): Cognitive test abnormalities start to appear, despite the ability to perform daily activities. 5-10% of people in this category progress annually to dementia. 4. Phase 4 (Dementia): This phase is marked by significant difficulty and impairment with daily tasks, requiring immediate care and intervention. Three Major Contributors to Alzheimer’s & Cognitive Decline: ● Energetics: Includes poor blood flow, oxygenation, mitochondrial function, and metabolic flexibility (ketones and glucose usage). ● Inflammation: Chronic inflammation drives amyloid production and brain degeneration. ● Toxins: Includes inorganics (e.g., mercury), organics (e.g., pesticides), and biotoxins (e.g., mold toxins). Tests to Diagnose and Understand Alzheimer’s: ● "If You Have It" Tests: ○ p-tau217: Early Alzheimer’s signaling ○ GFAP: Inflammation and repair in the brain ○ NfL: Neuronal damage from various causes ○ Aβ42/40 Ratio: Indicates amyloid plaque buildup ● "Why You Have It" Tests: ○ Metabolic panels, complete blood counts, and toxin screens (e.g., mercury, mycotoxins, and glyphosate) ○ Sleep studies to detect apnea and low oxygenation ○ Pathogen screens for viruses, tick-borne illnesses, and gut/oral health issues ○ Hormone levels, especially estradiol and progesterone during menopause Genetic testing (e.g., APOE, TREM2) and epigenetics for biological age assessment Prevention and Reversal Protocol ● Diet: ○ Plant-rich, mildly ketogenic diet with healthy fats, fiber, and omega-3s ○ Avoid grains, dairy, simple carbs; include healthy fats, fiber, and fermented foods ● Exercise: ○ Aerobic and strength training for improved oxygenation and insulin sensitivity ○ Minimum of 4-6 days per week ● Sleep: ○ 7-9 hours per night with good oxygenation (94-99% saturation). ○ Sufficient REM and deep sleep ○ Address issues like sleep apnea ● Stress Management: ○ Techniques like meditation, yoga, and nature walks to improve heart rate variability ● Brain Stimulation: ○ Cognitive training, photobiomodulation, and nerve growth factor enhancement ● Detoxification: ○ Eat a high-fiber diet ○ Sauna to help remove toxins ○ Identify and treat infections and mold exposures ○ Drink filtered water ● Key Supplements: ○ Resolvins: Reduce inflammation ○ Modified Citrus Pectin: Addresses inflammatory response ○ Whole Coffee Fruit Extract: Boosts BDNF (brain-derived neurotrophic factor) ○ Omega-3s (DHA and EPA): Support synapse formation and reduce inflammation ○ Vitamin D3: Essential for synapse formation ○ Nattokinase: Reduces risk of microinfarcts and thrombosis ○ Urolithin A: Helps recycle mitochondria ○ PQQ: Promotes mitochondrial production Other Considerations ● Fasting and Ketosis: ○ Promotes insulin sensitivity and metabolic flexibility ○ Use with caution for individuals who are underweight or frail ● Infections and Pathogens: ○ Addresses chronic infections (e.g., Lyme disease, herpes viruses, mold-related issues). ● Dental and Gut Health: ○ Resolve abscesses and optimize microbiome health. Sustained Improvement Over Time: ● Cognitive improvements can be maintained for over 10 years with continued optimization ● Secondary declines can occur but are often reversible by identifying and addressing new contributors Role of Personalized Protocols: ● Combining a plant-rich ketogenic diet, detoxification, stress reduction, and brain training yields the best results ● Developing a personal support system and/or utilizing a health coach will improve outcomes Day 4 Summary from Alzheimer’s is Now Optional How Clinical Trials Prove Cognitive Decline Can Be Reversed KEY TAKEAWAYS Study link: Sustained Cognitive Improvement in Alzheimer’s Disease Patients Following a Precision Medicine Protocol: Case Series The Precision Medicine Approach: ● This trial focused on identifying and treating the root causes of Alzheimer’s and MCI rather than using a one-size-fits-all treatment ● Unlike traditional treatments, which use standardized drugs, this trial personalized interventions based on each patient's unique contributors to cognitive decline. The study demonstrated significant improvements in cognition and sustained benefits over several years. ● Contributors like toxins, pathogens, genetics, and nutrient deficiencies were targeted for each participant. ● Compared outcomes to historical data of typical Alzheimer’s progression. Groundbreaking Clinical Trial: ● The 2022 study in the Journal of Alzheimer’s Disease involved 25 participants in advanced stages (MCI and dementia). ● Participants were 25 individuals in phases 3 and 4 of cognitive decline (MCI or early dementia). Baseline MoCA (Montreal Cognitive Assessment) scores were 19+ (out of 30). Tests and Metrics: ● MOCA (Montreal Cognitive Assessment) and CNS Vital Signs: Cognitive performance tracking ● MRI with Volumetrics: Brain volume changes, particularly gray matter and hippocampal volume ● Inflammatory Markers: hs-CRP, TGF-beta1, and MMP9 to detect systemic inflammation ● Mycotoxin Testing: Urinary mycotoxins, such as ochratoxin A, for identifying toxin exposures ● Sleep Studies: Diagnosing and treating sleep apnea, which significantly impacts cognition Results: ● Cognition: 84% improved cognitive scores, with MoCA scores improving in 76% of participants. CNS Vital Signs scores improved significantly. ● Brain Metrics: Brain MRIs revealed increased gray matter and reduced hippocampal volume loss compared to normal aging; hippocampal volume decline slowed significantly. ● Metabolism: Inflammation, insulin resistance, and lipid profiles improved. ● Partner Reports: Statistically significant improvements in participants' daily functioning as observed by caregivers. Patient Case Study (68-year-old woman): ● Initial symptoms: Cognitive errors, depression, and memory lapses (e.g., forgetting to pick up grandchildren). ● Diagnosed with MCI due to Alzheimer's disease and significant mycotoxin exposure. ○ Failed VCS (Visual Contrast Sensitivity) ○ C4a (measures the level of C4a protein) – 7990 ○ TGF-b1 (Human Transforming Growth Factor beta 1 test) – 4460 ○ MMP-9 (Matrix Metalloproteinase) – 497 ○ Urinary mycotoxins increased (OTA, MPA, citrinin) ○ MARCoNS+ (indicates antibiotic-resistant staph infection) ○ hs-CRP (assess inflammation) – 1.1 ○ Triglycerides – 29 ○ Zinc – 49 ● After a personalized protocol (ketogenic diet, detox, and targeted treatments), her: ○ MoCA score improved from 24 to a perfect 30 ○ Hippocampal volume increased significantly ● She sustained improvements for six years but experienced a mild decline due to new issues (e.g., previously undiagnosed sleep apnea, new mycotoxin exposure). After addressing these, her cognitive performance reached an all-time high. Day 5 Summary from Alzheimer’s is Now Optional Causes, Treatments, and Hope for Parkinson’s, Lewy Body Disease, and MSA KEY TAKEAWAYS Understanding Neurodegenerative Diseases: ● Parkinson’s disease, Lewy body disease, and multiple system atrophy (MSA) share common drivers like toxins, infections, and mitochondrial dysfunction. ● Key proteins like alpha-synuclein, similar to amyloid in Alzheimer’s, play an antimicrobial role but can accumulate and disrupt normal brain function. ● The mechanism for neurodegenerative decline is driven by the body's response to toxins, pathogens, and mitochondrial dysfunction. In Parkinsons, for example: ○ Alpha-synuclein proteins aggregate as a defense mechanism but result in neuronal damage ○ Affects the nigrostriatal pathway (a brain circuit responsible for controlling voluntary movements and body postural balance), leading to motor modulation deficits Early Warning Signs & Symptoms of Parkinson’s: ● Loss of smell, chronic constipation, and REM Behavioral Disturbance (RBD) can appear up to 10 years before motor symptoms. ● Loss of dopamine production causes tremors, rigidity, slow movement, and instability. ● Lewy body disease often involves cognitive decline, visual hallucinations, and Parkinsonism-like motor issues. Major Contributors to Parkinson’s: ● Toxins: Organic toxins like trichloroethylene, paraquat, and Agent Orange are major risk factors ● Mitochondrial Dysfunction: Loss of mitochondrial complex I function leads to low energy states and motor dysfunction ● Chronic Infections: Microbes can trigger immune responses, causing alpha-synuclein accumulation Tests and Diagnostics: ● MRI scans to detect brain changes in the nigrostriatal pathway ● Toxin exposure panels for organic and biotoxins ● Gut and oral microbiome assessments to identify imbalances and pathogens Effective Treatments and Strategies: ● Medication: Sinemet (L-DOPA), bromocriptine, and selegiline help increase dopamine through different mechanisms. ● Supplements and Support: ○ PQQ: Increases mitochondrial numbers ○ Urolithin A: Promotes mitochondrial recycling ○ Mucuna pruriens: Boosts dopamine naturally ○ Glutathione and Sulforaphane: Enhance detoxification ● Methylene Blue: Bypasses mitochondrial complex I dysfunction to restore energy ● Address Root Causes: ○ Identify and mitigate toxin exposures ○ Improve mitochondrial function ○ Detox strategies: Sauna therapy, cruciferous vegetables, glutathione supplementation ● Enhance Brain Function: ○ Exercise: Stimulates neurotrophic factors (a family of growth factors that modulate cellular growth, survival, and differentiation) ○ Sleep optimization and stress reduction ○ Brain stimulation / brain exercises ● Supplements ○ Pyrroloquinoline quinone (PQQ), Urolithin A, CoQ10, vitamin B6, and methylene blue ● To Increase dopamine: ○ Mucuna pruriens, Sinemet, Bromocriptine, Selegiline ● Gut Health: ○ Focus on microbiome restoration (e.g., fecal transplants) Lifestyle Interventions: ● Regular exercise, which increases GDNF (glial-derived neurotrophic factor) to support motor neurons ● A plant-rich diet with cruciferous vegetables to support detoxification and gut health ● Fasting and senolytics (like Fisetin) to reduce senescent cells and promote healthy cell turnover Advanced Therapies: ● Intravenous glutathione to boost toxin removal ● Plasma exchange for severe toxin cases ● Adipose-derived regenerative cells (stem cell therapy) to support neuronal repair ● Stem cell therapies and senescent cell reduction Comparison Between Alzheimer’s and Parkinson’s: ● Both involve the body's response to insults (toxins, pathogens). ● Key difference: Alzheimer's centers on memory and cognition, while Parkinson’s impacts motor functions. Both Alzheimer's and Parkinson’s are not merely conditions of misfolded proteins but systemic responses to various insults. Identifying and addressing the root causes allows for meaningful prevention, reversal, and long-term management of these neurodegenerative diseases. Day 6 Summary from Alzheimer’s is Now Optional Vascular Dementia and Its Connection to Alzheimer’s KEY TAKEAWAYS ● Understanding Vascular Dementia: ○ Vascular dementia occurs due to damage from small vessel occlusions (blockages), leading to reduced blood flow and oxygenation in the brain ○ It often overlaps with Alzheimer’s disease, as both involve vascular damage and inflammation ● Diagnostic Tools: ○ MRI with Fazekas Scoring: Identifies the severity of white matter abnormalities ○ p-tau217 Test: Detects potential Alzheimer’s components in cases with mixed dementia ● Common Contributors & Causes: ○ Hypertension (high blood pressure): Damages vessels and leads to occlusions ○ Type 2 Diabetes and Insulin Resistance: Increase vascular risks ○ Inflammation: Triggered by factors like mold toxins, lupus, or infections ○ Thrombosis: Tendency for blood clots to form due to hypercoagulable states (abnormal coagulation), sepsis, or amyloid buildup ● New Approach to Treatment: ○ Focus on root causes, identifying specific contributors like inflammation, toxins, or gut health issues ○ Personalized protocols addressing insulin resistance, inflammation, and vascular health ● Key Treatments and Strategies: ○ Reduce Clotting: Use nattokinase, lumbrokinase, or Pycnogenol to lower thrombotic tendencies ○ Dilate Blood Vessels: Boost nitric oxide with beetroot juice, L-arginine, or supplements like Neo40 or SuperBeets ○ Improve Blood Flow and Oxygenation: ■ EWOT (Exercise with Oxygen Therapy): Combines active exercise with increased oxygen delivery ■ HBOT (Hyperbaric Oxygen Therapy): Delivers high levels of oxygen to improve brain health ○ Target Inflammation: Use supplements like resolvins, omega-3s, curcumin, or PectaSol to reduce vessel inflammation ● Lifestyle Interventions: ○ Exercise: Increases blood flow and improves vascular health ○ Sleep and Stress Management: Reduce contributing factors to vessel damage ○ Diet: A plant-rich diet with anti-inflammatory and detoxifying foods supports vascular and cognitive health ● Overlap with Alzheimer’s Disease: ○ Many individuals have a mix of vascular and Alzheimer’s-related dementia, emphasizing the importance of addressing both vascular health and amyloid-related pathways ● Advanced Therapies: ○ Treatments like hyperbaric oxygen and nitric oxide boosters offer promising results for improving vascular dementia outcomes ● Key Goals: ○ Prevent vessel occlusion, improve blood flow, and ensure oxygenation to the brain for better outcomes Day 7 Summary from Alzheimer’s is Now Optional Macular Degeneration and Its Connection to Cognitive Decline KEY TAKEAWAYS Age-related macular degeneration (AMD) is the most common cause of visual loss in adults over 40. Overview: ● AMD is more common than Alzheimer's, Parkinson's, or vascular dementia. ● It results from a mismatch between the metabolic demand of the macula (the retina's most metabolically active area) and the support it receives. ● Two types: ○ Dry AMD: Early stage with insufficient blood flow and nutrient support ○ Wet AMD: Advanced stage where abnormal blood vessels grow and bleed in response to tissue demands Causes and Risk Factors: ● Lifestyle Factors: Excess blue light exposure, smoking, poor diet, and sleep apnea ● Health Conditions: Inflammation, type 2 diabetes, very high HDL, and poor mitochondrial function ● Environmental Toxins: Air pollution, mycotoxins, and secondhand smoke ● Genetics: APOE2 allele confers increased risk and APOE4 confers reduced risk (the opposite from Alzheimer’s) Diagnosis: ● Early Detection: ○ Changes in dark adaptation time (e.g. difficulty adjusting from light to dark) ○ Presence of "Drusen" (yellow deposits) seen in retinal imaging ○ Functional tests like visual acuity and the Amsler grid Treatment Approaches: 1. Optimize Supply: ○ Improve blood flow and oxygenation via nitric oxide supplements (e.g., beetroot juice) and therapies like hyperbaric oxygen therapy or exercise with oxygen therapy ○ Enhance mitochondrial function with supplements (e.g., nicotinamide riboside, CoQ10, acetyl-L-carnitine) ○ Ensure adequate nutrients (e.g., omega-3s, lutein, zeaxanthin, curcumin, zinc) 2. Reduce Demand: ○ Limit blue light exposure (e.g., blue light blockers) and encourage red light therapy to aid in healing ○ Address sleep apnea with CPAP or BiPAP therapy ○ Reduce metabolic strain by maintaining insulin sensitivity and promoting ketosis 3. Address Inflammation and Toxins: ○ Use anti-inflammatories like omega-3s and curcumin ○ Treat mold-related toxins and use HEPA filters to improve air quality 4. Early Interventions: ○ Identify AMD early and prevent progression from dry to wet AMD ○ Focus on metabolic flexibility and lifestyle changes to reduce risk factors Emerging Therapies: ● Red Light Therapy: Early studies suggest it may repair damage caused by blue light ● Stem Cell Therapy: Potential for advanced cases Study and Research: ● The Arc Project: Studies AMD along with other neurodegenerative diseases by addressing the supply-demand mismatch in neural subsystems. Goals: ● Improve early detection and functional outcomes ● Reduce the need for invasive treatments like eye injections for wet AMD ● Leverage lifestyle changes and targeted therapies to manage AMD effectively Day 8 Summary from Alzheimer’s is Now Optional The Future of Neurodegenerative Diseases KEY TAKEAWAYS ● Neurodegenerative Disease Paradigm Shift: Conditions like Alzheimer’s, Parkinson’s, and vascular dementia are being redefined as network insufficiencies rather than untreatable diseases. Addressing root causes like inflammation, toxins, and metabolic imbalance can lead to prevention and reversal. ● Advances in Early Detection: New biomarkers like p-tau217, GFAP, and NfL enable early and accurate identification of cognitive decline, allowing interventions at the earliest stages for better outcomes. ● The Role of Precision Medicine: Personalized treatment plans tailored to the individual’s unique contributors to neurodegeneration—such as toxins, genetics, and lifestyle—have shown significant success. In one study by Dr. Bredesen, 84% of trial participants improved cognition. ● Extending Brain Span and Health Span: Innovations in brain health are making it possible to maintain youthful brain function for a lifetime, reducing the global burden of neurodegenerative diseases. ● The Rise of Assisted Living Transformation: Facilities like Marama are proving that assisted living can become a place of recovery and improvement, with residents stabilizing or regaining independence. ● Application of AI and Big Data: Artificial intelligence is revolutionizing the analysis of large datasets, identifying critical contributors to neurodegeneration and optimizing personalized treatment protocols. ● Diet and Lifestyle Integration: Plant-rich, mildly ketogenic diets and anti-inflammatory strategies are foundational in supporting brain health and preventing disease progression. ● Personalized Brain Health Programs: Institutions like the Pacific Neuroscience Institute are setting new standards in brain health, offering comprehensive evaluation and precision treatments tailored to individuals. ● A Future of Cognitive Wellness: The vision for the future includes accessible prevention, better outcomes, and a global reduction in neurodegenerative diseases, empowering individuals to enjoy long and vibrant lives. THE FUTURE OF BRAIN HEALTH IS BRIGHT. Over the past sessions, we’ve explored a revolutionary approach to understanding, preventing, and reversing neurodegenerative diseases like Alzheimer’s and Parkinson’s. Here are the key takeaways and next steps to empower your lifelong brain health journey: A New Paradigm for Neurodegeneration: ○ Neurodegenerative diseases result from a combination of factors, including toxins, chronic infections, inflammation, and metabolic imbalances. ○ Proteins like amyloid and alpha-synuclein are not the root cause but rather protective responses to these insults. The Importance of Early Detection: ○ Conditions like Alzheimer’s and Parkinson’s progress through distinct phases, often starting decades before symptoms appear. ○ Early tests, such as biomarkers for amyloid and tau or assessments for mitochondrial function, allow for proactive intervention. Personalized Medicine Works: ○ Precision protocols that target the root causes of disease—including detoxification, mitochondrial support, and lifestyle changes—have led to dramatic and sustained improvements in thousands of patients. ○ Case studies show the power of identifying and treating specific contributors, such as toxins, sleep apnea, and mycotoxins. Core Strategies for Brain Health: ○ Adopt a plant-rich, mildly ketogenic diet, exercise regularly, and optimize sleep. ○ Manage stress, support detoxification, and use targeted supplements to improve mitochondrial function and reduce inflammation. A Future of Hope: ○ Advances in research and treatments make neurodegenerative diseases preventable, treatable, and reversible for many. ○ With a personalized, root-cause approach, the 21st century offers unprecedented tools to preserve and restore brain health.

Just chill, relax, take it easy. Don’t let things stress you out…. If it was only that simple, right? Stress is the one constant in all our lives. It can be insidious loops in our minds or unconscious thought patterns. For this blog, I wanted to talk about stress and how it affects every aspect of our life. Stress management is a major component to fixing a cascade of health-related illnesses, it’s a major health topic and worth exploring. Did you know that 70% of doctor’s office visits are related to stress in some form or another? Stress can cause depression, overeating physical symptoms such as high blood pressure, mitochondria inflammation, heart disease, cancer, and numerous other health issues. Stress response was developed as a way of survival when we would need to run from a lion or bear or be ready to fight. It comes from our fight or flight process in our brain. Modern society seems to be on edge, with triggers lurking in everyday situations like traffic jams, home security concerns, family disagreements, workplace conflicts, and the enduring pain of loss or separation. These stressors significantly shape our health profile. However, it's important to recognize that not all stress is detrimental. There's also 'good stress,' like the rush of adrenaline that sharpens your reflexes when you need to swiftly change lanes on the freeway, which serves as a protective mechanism before dissipating. What happens in society today though, is that we are bombarded all the time not only with what's physically around us but what’s virtually around us; notifications on our phone, text messages, social media posts and probably the worst is the news media and their constant barrage of negativity. We might not be able to control what is circling around us between family, friends, society, community, and the world at large. The only aspect we can manage is how we respond to stressors, and fortunately, there's a variety of stress-reduction methods out there. It's all about finding what clicks for you, as everyone's different. It's key to develop a stress-relief process that you actually look forward to. Here are a few ideas to consider. I have friends who are passionate about fishing; they find their bliss in the stream. Others enjoy golf, reveling in the game and the camaraderie as they hit balls and socialize. Then there are those who adore gardening, and I share this love. Being in my garden, watching my flowers and vegetables thrive, instills a sense of tranquility in me. Digging my hands into the soil and designing new sections of my landscape is a true stress reliever, at least until I spot aphids and other pests attacking my vegetables, which inevitably raises my cortisol levels. Many find cooking to be a soothing activity, that is how they take care of others and show their talents and creativity. I personally love self-care like getting a massage or taking hot baths with essential oils and relaxing episome salts. My daughter excels at meditation. She can immerse herself in silence for hours, honing her energy healing skills. While some find meditation stressful, overwhelmed by their swirling thoughts, unable to quiet their minds, meditation is not about silencing thoughts. It's about acknowledging and releasing them, refocusing on breath work. In stressful moments, I notice my breathing becomes shallow. We often hold our breath when we should be taking deeper, slower breaths to truly experience the calming effect of the process. I find yoga to be a very relaxing activity; it's a time when I can synchronize my mind and body in a free flow, allowing energy to circulate within me. Exercise is a form of stress on the body, but it's beneficial stress. It involves breaking down muscle fibers to rebuild them stronger, yet it's crucial for the muscles to rest and recover before being exerted again. Many of my friends are avid runners, finding stress relief in running, weightlifting, and other forms of physical activity. Gathering with friends to talk, laugh, and socialize is another excellent stress reliever, with laughter being one of the best. Additionally, hot and cold therapy serves as another positive stressor, aiding in the release of toxins and accumulated chemicals in the body. Here's an overview of the processes occurring within your body: The hypothalamic-pituitary-adrenal (HPA) axis, which regulates the stress response, relies on proper mitochondrial function. Mitochondrial dysfunction can disrupt the regulation of the HPA axis, leading to an altered stress response. This can contribute to depression and other chemical reactions within your body. Prolonged stress may cause mitochondrial dysfunction through various mechanisms. One such mechanism is the activation of cortisol release, a steroid hormone that can directly damage mitochondria. Cortisol is known to suppress the expression of genes involved in creating new mitochondria, thereby reducing the number of mitochondria in cells and leading to decreased energy production. Additionally, excess cortisol can increase free radicals, partly by inhibiting the production of antioxidants. Numerous instances demonstrate that stress alone can elevate your glucose levels, independent of diet. This occurs because cortisol, the primary stress hormone, instructs the liver to break down stored glucose and release it into the bloodstream. This energizes the muscles in preparation for a threat, as our bodies are designed to be agile and ready for quick physical action. However, in today's world, stressors such as arguments, emails, car horns, and phone notifications activate stress responses that seldom necessitate muscular activity. Consequently, the released glucose remains in our bloodstream, doing more harm than good. A continuous glucose monitor can serve as a potent tool, teaching us about the impact of stress on our metabolic health and encouraging us to manage acute stress through healthy practices such as deep breathing. Indeed, intense, acute stress and chronic stress triggers are indicative of negative energy. A study on chronic inflammation in mice revealed that merely six hours of acute stress can lead to a swift mobilization of the immune system, with an increase in the concentration of inflammatory markers—specific immune chemicals involved in the initial response to infections and wounds, as well as in the gene expression of pathways related to the migration of immune cells. Stressful thoughts can trigger neuroinflammation, which is inflammation of the brain that leads to metabolic dysfunction and increases the risk of diseases like depression and neurodegeneration. This inflammation affects not just the brain but the entire body, activating the stress response system and the sympathetic nervous system. Overactivation of this system can cause insulin resistance, hyperglycemia, and the spread of inflammatory cells, worsening energy levels throughout the body. Prolonged psychological stress, such as from child abuse, is linked to higher levels of inflammatory cytokines. Inflammation can disrupt energy by blocking glucose channels and insulin signals, and by promoting the release of free fatty acids, which contribute to insulin resistance. Healing our brain is crucial, and regardless of past experiences or current world events, finding a sense of safety is key to health. This sense of safety can be developed within our minds and bodies through intentional practice. Addressing chronic stress, triggers, and life traumas is a lifelong journey without a universal solution. The initial step is recognizing their impact on our health. Subsequently, we must enhance our body's physical structure and function through dietary and lifestyle strategies that foster a biological state conducive to mental health. This includes adopting practices that manage and heal stressors, traumas, and limiting thought patterns, thereby improving our metabolic health. While healthy eating, adequate sleep, and exercise may seem insignificant in the face of existential dread or depression, they are crucial. Committing to at least 150 minutes of elevated heart rate activity weekly and adhering to principles of clean, healthy eating can lead to noticeable improvements, equipping your brain to better handle life's stresses. Getting enough sleep can transform your outlook on the world, making it seem more inspiring. Concentrate on establishing good habits and the positive outcomes will follow. A great initial move is to pick a healthy and motivating activity and just try it out; after all, small victories pave the way for bigger triumphs. Here is my summary of 15 strategies that may be beneficial from the book "Good Energy" by Dr. Casey Means and her brother Calley Means. 1. Form relationships with a mental health therapist, coach or counselor. 2. Monitoring your heart rate variability (HRV) can be beneficial for your health. Consider using wearable devices such as Whoop, Apple Watch, Fitbit, or Oura to track and enhance it. There are numerous monitors available that can assist with this. 3. Practicing breath work is an effective method to stimulate the vagus nerve and activate the parasympathetic nervous system, which oversees the body's rest and digest functions. Numerous guided videos and apps are available for practicing mindful meditation. Engaging in consistent mindfulness meditation for eight weeks, with daily sessions as brief as 10 minutes, has been demonstrated to substantially reduce various metabolic biomarkers, such as triglycerides and blood sugar levels, while also enhancing mood and alleviating anxiety and depression. 4. Mindful movement practices such as Yoga, Tai Chi, or Qi Gong have been shown to benefit both physical and mental well-being. Research indicates that these body-mind interventions can alleviate depression, anxiety, and stress. Additionally, they enhance the activity of the parasympathetic nervous system, which can lower cortisol levels, reduce inflammation, and alter gene expression, thereby positively affecting metabolic concerns. 5. Research indicates that spending time in nature can significantly reduce stress hormones and enhance the parasympathetic nervous system, improving mood. Even a visit to a city park can have a noticeable effect on health and stress levels. 6. Exploring inspirational and thought-provoking books on mindset, trauma, and the human condition can be transformative. There's a wealth of excellent literature on mental health, mindset, and redefining one's relationship with stress. Titles like 'The Trauma Mindset,' 'A Return to Love,' 'Untethered Soul,' 'How to Do the Work,' and 'Brain Energy' are just a few examples. Additionally, there are numerous authors, poets, and podcasts available for further insight and inspiration. 7. Consider aromatherapy; clinical research indicates that natural scents can significantly trigger relaxation. Lavender oil, in particular, is well-researched and highly effective in reducing stress and aiding sleep, as detailed in the peer-reviewed article "Lavender and the Nervous System." Apply a few drops of lavender essential oil to your hands, bring them to your face, and take deep breaths to experience its benefits. 8. Writing can be a powerful tool when you're feeling overwhelmed or stuck. Try setting a timer for five minutes and just write about whatever is bothering you. It's not only a fantastic outlet for creativity but also a means to gain perspective. Regular writing can help reduce stress, enhance cognitive functions, and even alleviate anxiety and inflammation-related conditions. Keeping a journal and concentrating on positive emotions such as gratitude or the ways others have supported you can significantly lessen mental distress, especially for those dealing with medical conditions and anxiety. 9. Consciously cultivating gratitude by acknowledging abundance daily enhances my well-being. On my best days, I begin with a blank sheet of paper and jot down everything I'm thankful for. This practice fosters a deep sense of abundance, which soothes me and enables me to operate from a position of security instead of fear. 10. Taking a walk, intentionally focusing on finding the aww that is around you, clouds, trees, flowers anything that brings you a sense of peace 11. Practice acts of self-love, be mindful of negative self-talk and find ways to become your biggest supporter and the greatest love of your life 12. Be less busy, embrace Jomo (the joy of missing out). Get comfortable with periods of unstructured time alone without constant distractions. Find pleasure in saying “no” when you aren’t completely excited about a particular activity or event. 13. Fostering community is essential: Loneliness, experienced frequently by one-third of US adults, can adversely affect metabolic health, as social connections are evolutionarily crucial for survival. Loneliness may have developed as a warning signal, akin to hunger or thirst. Engage with friends or family or initiate a chat with a stranger—such interactions could be mutually beneficial. 14. Committing to a digital detox is beneficial: Research indicates that excessive smartphone use is linked to adverse psychiatric, cognitive, and emotional effects, altering brain function. Decreasing smartphone usage by merely one hour daily can reduce symptoms of depression and anxiety, enhancing overall life satisfaction. 15. Consider psilocybin-assisted therapy. A 2016 Johns Hopkins study revealed that 67% of participants rated their experience with psilocybin as either the single most meaningful experience or among the top five most meaningful experiences of their lives, comparable to events like the birth of a first child or the death of a parent. It's hard to imagine a more significant research discovery. Similarly, a recent UCSF study indicated that individuals with severe PTSD who received MDMA during therapy showed a significantly greater reduction in symptom severity compared to those who underwent talk therapy alone. Stress is a consequence of our ability to self-regulate emotional states. It is both Good and Bad at the same time, it’s in our control how we view and manage our responses. You have the power to change those reactions. With Love Be Well Susan Lee

In the next few blogs, we will start down the pathway of the Health Foundation…but first I thought we should start with a few topics many of us face daily. Some traits are ingrained from childhood, others stem from experiences later in life. These are the subconscious characteristics we carry with us. Perfectionism and procrastination…Two words that can potentially hold us back from finding our path to well-being. This second blog was a hard one to get started. I was procrastinating because I wanted it to be perfect. We all go down this pathway, it’s in the realization and acknowledgement of catching yourself that we can find peace and self-acceptance. Perfectionism often involves spending considerable time concerned with others' opinions about oneself, one's home, or family situation. This preoccupation can be a barrier to pursuing a life filled with joy and satisfaction. I first encountered the concept of perfectionism as a child, believing that love was conditional upon my achievements. I thought that excelling in school or surpassing my older sisters in beauty and intelligence would earn me the attention I desired from my family. During my preteen years, this belief only intensified my self-criticism and the sense of inadequacy, further harming an already delicate teenage ego. This started me down a path of unhealthy practices, taking diet pills and self-loathing. Thinking I was not pretty enough, not skinny enough and often, not smart enough. Spending time pouring over beauty magazines, was my equivalent of what teens face now with social media. This feeds an unhealthy obsession with comparison to others, and now with a digital twist of filters and AI. Many of these childhood experiences and thoughts follow us into adulthood. We tend to focus outwardly when in reality it’s the inner work that will bring us clarity and focus. I desired plastic surgery, to fix this and that and was a fan of the show Extreme Makeover. If only, was a thought that ran through my mind. I turned to the next best thing, and again worked on improving my life from the outside. I obsessively worked on our home, remodeling, painting, and designing - activities I love. Yet, in retrospect, I realize I was attempting to fill that void, the inner belief that I wasn't enough. This was during the HGTV and Fixer Upper phase, the home improvement phenomenon was rampant. We occasionally had guests over; the obsessive cleaning and organizing I felt I had to do before guest came, felt overwhelming at times. Our home always felt "unfinished"—the hallway needed painting, or something required a redo or a touch-up. It was an endless cycle of projects. Nothing ever seemed sufficient or perfect. The costs exceeded our budget, and the sense of achievement was transient. Over time, I've realized this urge was to fill an inner void and have sought to understand and now recognize its origins. I will admit that working on decluttering and building comfortable surroundings was a catalyst for doing my inner perspective work; it was a long road, looking back now, worth the effort. When we purchased our 1909 craftsman Victorian home, I told my husband “it was perfect as is, fully renovated, he wouldn’t have to do a thing.” However, during the walk-through, I already envisioned the updates and changes I wanted to make. Living in this 115-year-old home, with all its original woodwork and charming quirks, I've come to appreciate its imperfect beauty. The signs of 115 years of life and love that have passed within these walls taught me to embrace its imperfections. There's a beauty and joy, a comforting welcome that greets me as I enter this home. I realize now it’s not the house, it’s the letting go of perfectionism that has changed…and yes, a few updates. Perhaps with age comes the ability to accept our imperfections, our wrinkles, our weight, and our distinctive quirks. There is a lightness in embracing who we are, a sense of peace and acceptance. Being healthy is not about perfection; it's about mindset to improve how we feel and the energy we have. Procrastination often mirrors perfectionism. It's a method of dodging tasks you know should be tackled, yet you find reasons to avoid them. Thoughts like "I'll start next week," "I'll do it on Monday," or "Once I achieve this goal, I'll be happy," are common. "I'll launch that podcast when I have enough followers," or "I'll apply for that job once I lose weight," are examples of delaying ambitions because we believe we're not in the ideal relationship, don't have the perfect body, friends, city, job, or whatever else we think must be perfect for us to realize our full potential. Embarking on a journey toward personal well-being involves a process. It requires self-exploration to understand what impedes you from setting or attaining your goals and achieving an improved state of wellness for yourself. What I can say with 100% certainty is that you are worth it, you are perfect in God‘s eyes…You are enough! Now is the perfect moment to recognize your inner power and radiance, let’s get you moving in a direction of acceptance, awareness self love, and the beautiful reality of who you are right here and now. Nourish ~Grow ~Bloom with me! With Love, Be Well Susan Lee Check out a few ideas below to help start this journey 7 Steps to Breaking the ‘Perfectionism, Procrastination, Paralysis’ Cycle Medically reviewed by Timothy J. Legg, PhD, PsyD— Written by Meagan Drillinger 1. Consciously lower the bar The first step to breaking that cycle is to recognize that often times, accomplishing tasks is a slow process, and an imperfect one at that — and that’s normal and totally okay. It won’t happen all at once. It’s okay to take your time. It’s okay to make mistakes (you can always go back and fix them later!). In other words, it’s okay to be human. It’s easy to forget this, though, when so many of the expectations we have of ourselves are lurking just below the surface, fueling our anxiety. 2. Keep your tasks bite-sized “Tackling perfectionism requires disrupting all-or-nothing thinking,” says Dr. McDowell. “For example, if you’re trying to get your inbox organized, it’s not going to help if you consider that as one single task. Figure out what the components of the task are, and take them in bite sizes.” Breaking down tasks into their smaller pieces not only makes them more manageable, but leads to more frequent feelings of accomplishment as you cross each one off your list. 3. Track your time It’s important to remember that when a task is looming over us and we’ve built it up to be a behemoth, we often overestimate the time it takes for us to complete it. When you think an anxiety-inducing task will take the entire day, you also tend to not schedule any time for self-care. “Balancing priorities is important,” says Dr. Supriya Blair, licensed clinical psychologist. “This is why we include time for social and self-care activities during our daily and weekly schedule. Holding oneself accountable to follow through on work and fun activities takes practice, patience, and self-compassion.” 4. Surround yourself with positive support Power in numbers! Tackling anything alone is more overwhelming than doing so with a support system. One of the best ways to get organized when you have anxiety is to partner up with a supportive, hardworking companion, whether it’s your significant other, friend, parent, or child. You can also reach out to a therapist or life coach to get some much-needed perspective. 5. Practice saying ‘no’ It’s impossible for one person to commit to absolutely everything, but we often feel the need to please everyone. Taking on too many responsibilities is a sure-fire way to become overwhelmed and to then fall into the similar self-destructive cycle. “Think about where you can streamline your schedule, delegate to others, or even say no to events and tasks that are not immediate or urgent,” says Angela Ficken, a psychotherapist who specializes in anxiety and OCD. 6. Use the reward system You’re never too old to reward yourself, and often setting up small rewards can be one of the most effective ways to motivate yourself to get organizational tasks done. “Focus on how you will feel when your home is organized and clean, how exciting and fun it can be to plan your wedding, how responsible you will feel when you complete your taxes,” says Dr. Nancy Irwin, a psychologist with Seasons in Malibu. “Then reward yourself for a job well done. Positive reinforcement ensures the next project can go as smoothly and informs you that you are bigger than the anxiety,” she says. 7. Incorporate mindfulness Staying in tune with your body and mindset as you practice breaking patterns can be extremely beneficial. Self check-ins are critical, especially if you’re prone to honing in on the smallest details. To avoid feeling overwhelmed, it’s important to take a step back to give yourself breaks and reminders. “Mindfulness is key,” says Ficken. “A relatively easy mindfulness skill is to take yourself outside for a walk or to sit out on your stoop. Being out in the elements can be an easy visual and sensational cue to bring yourself into the present moment.” Keeping grounded is an important part of keeping your anxiety in check. Don’t hesitate to take a breather when you feel your anxiety building — your body and brain will thank you later! A Few Quotes…. “A flower does not think of competing with the flower next to it. It just blooms”~Zen Shin “Perfectionism is a twenty-ton shield we lug around thinking it will protect us when, in fact, it’s the thing that’s really preventing us from taking flight.” ~ Brené Brown “Perfectionism is not as much the desire for excellence, as it is the fear of failure couched in procrastination.” ~Dan Mille



